I find the physiology behind intuitive eating to be really fascinating. I love the concept of our bodies having a natural rhythm and an internal sense of regulation. Healing from my eating disorder and really committing myself to intuitive eating has been a really empowering experience for me. I know so much more about my body now than I did ten years ago. Part of that awareness has come from studying every detail of the human body in school, but a lot of it has also come from years of practice in listening to my body’s own cues. Getting to know my own hunger and fullness, my need for rest, my threshold for stress, and how and when to move my body in a way that feels good has been an extremely empowering experience for me. Knowledge really is power!
More recently, I’ve been getting to know myself better by tuning into the natural changes that take place during my cycle. I’ll admit, for most of my life I preferred not to think about my period very much. I found it to be inconvenient and, at times, embarrassing. (We’ve all been there…) Once I got married, though, I started paying more attention to everything going on in relation to my cycle. At first it was for family planning purposes, but I slowly started to notice cyclic, predictable changes in my body that had nothing to do with “that” time of the month—energy levels, hunger patterns, motivation, introversion versus extroversion, and more. I found it super fascinating, especially when I started comparing those changes to the hormonal patterns I’d learned about in school.
In the same way that intuitive eating has helped me build trust with my body, learning about my cycle in a more personal way (rather than just reading a textbook) has helped me build trust with my body. It feels so good to know that everything is working as it should, and what to do if something seems amiss. If you’re interested in learning about that too, this post is for you!
Hormones and the HPATG Axis
If you remember from last week’s post, our monthly cycles begin and end in our brains. Part of the brain called the hypothalamus sends hormonal signals to the pituitary gland, triggering another hormone cascade that tells our reproductive organs what to do, and when. Although different circumstances can interfere with that communication axis, for the most part, the hormonal pathways work like this:
The main signals sent out by the pituitary gland are luteinizing hormone (LH) and follicle-stimulating hormone (FSH). These hormones travel through the blood stream to the ovaries, stimulating the production of estrogen and progesterone. These four hormones rise and fall in predictable patterns throughout the menstrual cycle to trigger ovulation, thicken the endometrial lining, and shed unused tissue if pregnancy doesn’t occur.
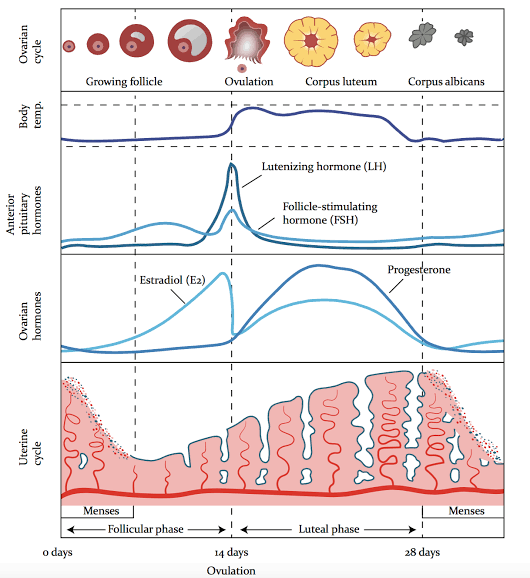
The menstrual cycle is divided into two main stages, the follicular phase and the luteal phase. Within those two phases we have two pretty noteworthy events (ovulation and menstruation), so I like to think of the cycle as having 4 phases, beginning with the first day of your period (cycle day 1 [CD 1]). Although the length of normal cycles can range anywhere from 21 to 35 days, most are around 28 days, so that’s the reference range I’ll be using in this post.
- Phase 1 (Menses [CD 1-7]): This is probably the part of your cycle you’re most familiar with: your period. When counting the days of the menstrual cycle, we count the first day of the cycle as the first day of a period. Some women experience light spotting in the days leading up to their period, but those days are counted as part of the luteal phase (phase 4). Cycle day 1 (or CD 1) is counted as the first full day of bleeding. Technically, the days of your period fall within the follicular phase, because they start the beginning of the hormonal processes that lead to menses in the following month’s cycle. In terms of your hormonal cycles, the formal end date of your period doesn’t matter so much as the first day of bleeding.
- Phase 2 (Follicular Phase [CD 1-13]): During this phase (yes, even starting on the first day of your period), your body is starting to prepare for next month’s period—or a possible pregnancy. The first day of the follicular phase, CD1, is the day when hormone levels are at their lowest. Estrogen and progesterone are at their minimum, and follicle-stimulating hormone (FSH) and luteinizing hormone (LH) are laying low, too. Over the course of the first week, FSH levels slowly start to rise, stimulating ovaries to slowly ramp up production of estrogen. The estrogen circulates throughout the body playing a number of different roles, but the most noteworthy action in terms of fertility takes place locally, at the ovary. When estrogen levels begin to rise, about 12-18 ovarian follicles start to ripen. Eventually, most of these follicles die off, and just one finishes the maturation process, an event that corresponds to the day when estrogen is at its highest. Estrogen production peaks at around days 11-13, then sharply falls. The pituitary gland senses this drop in estrogen through a feedback loop. Its response is to send out a surge of FSH paired with an even stronger surge of LH to trigger ovulation.
- Phase 3 (Ovulation [CD 14]): On the day of ovulation, the sharp rise of FSH and LH stimulates the mature ovarian follicle to burst open, releasing the egg. The egg travels down through the fallopian tube, and if unfertilized, dissolves within 24-36 hours. What’s left of the follicle collapses, becoming the corpus luteum, and begins producing progesterone, the dominant hormone of the luteal phase.
- Phase 4 (Luteal Phase [CD 14-28]): After ovulation, FSH and LH levels drop back down again, and hormones in general reach another realative low. Beginning with the day of ovulation, however, the corpus luteum takes over hormone production, secreting progesterone and some estrogen, which thicken the uterine lining to prepare for a possible pregnancy. Progesterone levels peak at about CD 21, followed by a gradual decline of both estrogen and progesterone. (Eventually the corpus luteum breaks down into the corpus albicans, eventually dissolving completely.) When the hormones levels bottom out, the menstrual lining begins to slough off and the cycle starts all over again.
Getting to know YOUR cycle
Women typically express an interest in their cycle when they start the process of trying for a baby. While unprotected sex technically could lead to a pregnancy at any point depending on each individual woman, there are really only 5-6 days each cycle that conception is really possible. These days correspond to the 5 days leading up to, and including, ovulation as well as the day after ovulation.
Fertile Days
These fertile days really depend on the lifespan of sperm. The actual union of sperm and egg can only take place on the day of ovulation and the 24-36 hours thereafter, until the egg dissolves. Sperm, however, can live up to five days in the uterus and fallopian tubes, waiting around for the egg to be released. In a 28 day cycle, these fertile would correspond to CD 10 through CD 15. Having unprotected sex on any other day corresponds to a very, very, very low chance of conception, and this awareness serves as the basis for Fertility Awareness Methods of family planning.
But of course, not every woman’s cycle lasts the textbook length of 28 days. In order to get to know you and your cycle, there are a number of personalized methods you can use.
Cycle Tracking Method #1: Hormone Testing
At-home urine hormone tests can be used to predict and confirm ovulation, and they’re pretty inexpensive. The testing procedure involves placing a urine dipstick into a sample of urine. If the hormone target is present in the urine, it will react with a reagent and bind to a dye strip—similarly to a home pregnancy test. Ovulation predictor test strips qualitatively measure levels of luteinizing hormone in the urine, and generally show a pale pink line on most days of the follicular phase. On the day of LH surge, the test strip will turn dark pink, indicating a sharp increase in the level of LH. This LH surge means that ovulation will likely take place within the next 24-48 hours. (Note: LH typically peaks in the afternoon, so afternoon urine tends to catch the LH surge better than morning urine.)
Affiliate Link: Ovulation Test Strips (LH)
In a very small percentage of women, the pituitary gland sends out a surge of LH, but the follicle fails to release an egg. Because of this, many women prefer to confirm that ovulation has taken place by testing for progesterone metabolites in the urine. During the luteal phase, as progesterone production ramps up, so do the levels of the breakdown products detectable via urine test strips. Progesterone test strips work similarly to ovulation predictor kids, except a second pink line showing up (in addition to the control line) indicates a negative test, and the absence of a line indicates a positive. (Note: progesterone test kits typically recommend testing the first morning urine.)
Affordability: Good. LH test strips each cost less than 50 cents each, but the downside (especially with ovulation predictor kits) is that you need to test every day—sometimes multiple times per day. (Progesterone test strips are a little pricier.) If you have no idea when you might be ovulating, using these strips regularly, or for multiple months in a row, can add up.
Ease: Excellent. Open, dip, read, move on.
Validity: High. The test is either positive, or it isn’t. When both the LH and progesterone tests are positive in a given month, there is a near-perfect likelihood that ovulation has taken place.
Accuracy: Pinpointing ovulation with urine test strips is not really possible. The LH surge simply means that ovulation will take place sometime in the next day or two. Progesterone test strips mean that it has taken place sometime in the week, give or take. Using urine strips alone would not be considered a reliable way to prevent pregnancy if you are tracking your cycle for contraceptive purposes.
Cycle Tracking Method #2: Basal Body Temperature
If you look back at the chart at the top of the post, you’ll see that the very top line corresponds to body temperature. Sometime throughout history, women realized that the menstrual cycle creates predictable changes in basal body temperature (BBT)—our core body temperature while at rest.
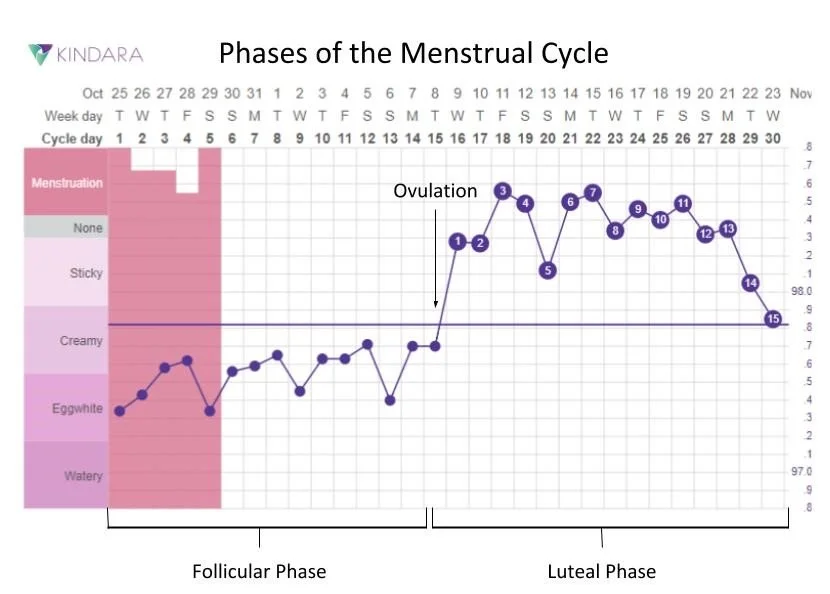
Throughout the follicular phase, our BBT is at its low point. The day after ovulation, it takes a sharp rise, usually of more than 0.2 degrees. This temperature rise is sustained until a few days before your period, when it slowly drops back down again. After tracking your BBT for a few cycles, you’ll have a pretty good idea of when you ovulate and when to expect your period, which can be helpful whether you’re trying to conceive, or altogether avoid pregnancy.
Affordability: Excellent. However, measuring BBT requires a more precise measurement than most at-home thermometers are capable of. In order to offer the level of precision needed for accurate monitoring, the thermometer needs to read more than two places past the decimal point. Thankfully, this method is popular enough that BBT thermometers are extremely affordable—less than $10. [Affiliate link: Basal Body Temperature Thermometer]
Ease: Medium. Basal body temperature readings are only valid if they are taken first thing after waking up, even before getting up to use the bathroom, get a drink of water, or anything else. The reading also must be taken after at least 3 hours of uninterrupted sleep. If you’re a restless sleeper, struggle to remember to take your temperature, or snooze abuse, this method might not be right for you.
Validity: Medium. BBT can easily get thrown off from things like illness, alcohol, sleeping next to a warm person, or even temperature changes in your bedroom. But when the conditions are right, BBT charting can be highly effective.
Accuracy: When done correctly, BBT charts are a highly accurate method for tracking fertility. The post-ovulatory temperature rise is a pretty clear indication that ovulation has successfully taken place.
An additional benefit of this method is that sometimes it can serve as an early method for detecting pregnancy. Many women experience an “implantation dip” about 6-12 days after ovulation, when the temperature drops around 0.3 degrees, and then rises back up again. If the temperature remains high and doesn’t start to drop off, as is the case before menstruation, this usually is an indicator of pregnancy, sometimes even earlier than a home pregnancy test.
Cycle Tracking Method #3: Tracking Cervical Mucus
This method is the most…intimate of all. It requires that you get really comfortable with yourself and your anatomy.
Vaginal discharge (AKA cervical mucus) is a normal part of female health. Significant changes in color or odor can indicate infections, but outside of these instances, clear, white, or pale yellow discharge is a predictable part of being a woman. Throughout the cycle, the texture and color of cervical mucus changes in predictable patterns:

To accurately assess your cervical mucus, you can wipe your vaginal area before urinating, and observe the tissue. Alternatively, with clean hands, you can insert a finger or two slightly inside your vagina and observe the color and texture between your fingers.
On days when cervical mucus is scant, fertility is low—meaning pregnancy is highly unlikely. But on days when cervical mucus is more abundant, and especially when slippery and watery in the days leading up to ovulation, fertility and chances of conception are very high. Typically in the few days leading up to ovulation, cervical mucus will become clearer and more abundant, resembling raw egg white. Not only do these days signify pending ovulation and a time frame in which sperm can survive, but the egg white cervical mucus (EWCM) actually serves to promote sperm survival. It contains high levels of water and nutrients, promoting sperm fertility as well as a nutritious environment to help them traverse the journey up through the fallopian tube to wait for an egg. If you’re trying to conceive, the days you notice EWCM are the days you and your partner should be getting busy.
Affordability: Excellent. All you need are your own two (clean) hands and/or some toilet paper.
Ease: Medium/Low. This method of cycle tracking requires a degree of personal intimacy and comfort that the other methods don’t. Learning how to differentiate among the different textures and quality of cervical mucus can also be really challenging during the first few months. It’s not as cut-and-dry of a method as taking your temperature or using a test strip.
Validity: Medium. The results are mixed with this method, as not all women follow quite the same patterns. For example, some women may produce low amounts of EWCM, making it difficult to identify fertile days.
Accuracy: Medium. When EWCM is present, chances of conception are high. However, for women trying to avoid pregnancy, tracking cervical mucus alone may not be sufficient to identify fertile days.
Cycle Tracking Method #4: Symptom Spotting
I’m listing this method last because it really shouldn’t be used as a method for pregnancy prevention, or even timing intercourse for conception. However, paying attention to your internal, bodily signals at different times of the month can give you valuable insight into your own body’s needs, informing your self-care routine throughout the month.
Menses: Letting Go
Most women tend to feel lethargic and less social during the first few days of their periods. Looking back at the rise and fall of hormones throughout the cycle, this totally makes sense. Estrogen and progesterone are at their all-time low during the first few days of your period, and low levels of these hormones are known to correspond to feelings of anxiety, depression, and fatigue.
I used to find this feeling extremely inconvenient, but as I gained knowledge of and trust in my body, I slowly came to recognize that things go so much better when I accept my natural design instead of trying to battle against what my body is doing. Menstruation is a natural part of life as a woman, and when I set aside my pride, I can see that this natural time of release and letting go can be really healthy depending on how I respond.
Many women (myself included) find that symptoms like cramps and breast tenderness are less severe when I accept my body’s invitation to slow down and rest. I tend to naturally feel more introverted and tired during the first few days of my period, and I’ve realized that I feel so much better if I don’t push myself to perform or be social, and take it easy with exercise. Instead of focusing on my productivity, I try to use this time to relax, reflect, and let my body go through its own process of restoration.
Follicular Phase: Estrogen for Energy
On a biochemical level, estrogen is an energizing hormone. As levels start to rise during the follicular phase, we tend to feel motivated, energetic, and productive. I personally find that intense exercise feels really good in my body throughout days 5-15 of my cycle, and I’m madly efficient when I work on things (like writing this monster of a blog post, for example…)
I also find that I’m much more willing to get things done around the house, participate in trips and social events, and tie up loose ends at work. While I don’t necessarily go so far as to make special plans during this time, the knowledge that I’m not always so energized allows me to have a little more grace on myself when I realize that my hormones have such a profound affect on that areas of my life.
Ovulation: Transition
I personally don’t notice any remarkable changes in my body or mind during ovulation, but many women report implantation cramping, breast tenderness, or light spotting on the day leading up to or day of ovulation. This can serve as another means for tracking your fertility if you find yourself with these sorts of symptoms.
Luteal Phase: Rest and Restore
Progresterone is the hormone responsible for PMS symptoms. As the corpus luteum starts to ramp up its secretion of progesterone, levels of fatigue, breast tenderness, cramping, irritability, and bloating tend to follow suit. Digestion slows way down, electrolyte levels fluctuate (leading to water retention), and mammary tissue starts to develop in the event of a possible pregnancy—leading to swelling and tenderness. Progesterone is also responsible for aches and pains, acne flare ups, constipation, and headaches…all the lovely symptoms we associate with PMS and early pregnancy.
As with the first days of my period, I tend to feel sluggish, tired, and sore during the last few days of my luteal phase. By tracking the symptoms of my own cycle, I’ve come to recognize that feeling slow and tired during exercise, mild tension headaches, and a predisposition to feel a little antisocial is normal for me. While I find these things to be a little inconvenient, they aren’t debilitating, and I generally feel pretty good when I respond appropriately to my body’s signals for rest. As it says in Ecclesiastes chapter 3, “For everything there is a season, a time for every activity under heaven. A time to be born and a time to die, […] A time to tear down and a time to build up. A time to cry and a time to laugh.”
To sum things up…
The female body is an incredible, awe-inspiring creation. I am truly amazed every time that I sit down and study the details of hormonal balance, the delicate web of connections between our hormones and our bodily systems, and the amazing miracle of pregnancy and birth. The beautiful, graceful way that everything works together inspires a deeper sense of respect for everything that my body is—and isn’t—and drives me to take self-care seriously so that I can continue to live a healthy, vibrant life.
If you’re struggling with your health—whether in terms of your fertility, hormonal balance, or something else—send me an email or fill out a contact form. I work with women with these concerns through all the time, and I’d love to help you, too.
10 thoughts on “Female Fertility 101 (Hormones, Cycle Tracking, and Getting to Know YOUR Body)”